Case Report
Case Report
An Atypical Variant of the Deltoid Muscle- A Case Report with Procedural Considerations
Chase Green1*, Bassam Ballout1 and Armando Rosales2
1Texas College of Osteopathic Medicine, University of North Texas Health Science Center, United States
2School of Biomedical Sciences, University of North Texas Health Science Center, United States
Chase Green, Texas College of Osteopathic Medicine, University of North Texas Health Science Center, 3500 Camp Bowie Blvd, Fort Worth, Texas, United States
Received Date:February 09, 2024; Published Date:February 20, 2024
Abstract
This case report describes an atypical deltoid variant discovered during cadaveric dissection of a middle-aged male donor. The bilateral spinal segments of the deltoid muscle (DM) were found to be encased in a distinctive fascial compartment, disconjugate from the normal morphology. The spinal segments were found to be innervated by a branch of the axillary nerve and perfused by a branch of the posterior circumflex humeral artery. Divergences from expected anatomy are important clinically in respect to surgical interventions, as correctly identifying in situ anatomy is essential for the accurate diagnosis and treatment of shoulder pathologies. Unexpected anatomical variations can cause unanticipated surgical delays, and the misidentification of in situ anatomy can be a cause for iatrogenic injury –both of which can increase the probability of unfavorable outcomes in the care of the surgical patient.
Keywords:Deltoid muscle; Variant; Fascia; Iatrogenic injury; Nerve injury; Axillary nerve block; Muscle flap; Shoulder surgery
Abbreviations:DM: Deltoid Muscle, GHJ: glenohumeral joint
Introduction
The DM is a complex, flat muscle that envelopes the entire shoulder girdle and contributes to multiple, competing movements of the upper limb. It is comprised of three functional segments with distinct tendonous attachments: the clavicular segment attaches from the inferior edge of the clavicle to the deltoid tuberosity of the humerus, the spinal segment from the lateral two-thirds of the scapular spine to the deltoid tuberosity, and the acromion segment from the acromion process to the deltoid tuberosity [1]. The DM is a complex primary abductor of the humerus, with functional segments that contribute to humeral flexion (anterior segment) and humeral extension (posterior segment). It is innervated by the axillary nerve derived from motor roots of C5-C6 as the terminal branch of the posterior of the brachial plexus [2]. The DM receives a dual blood supply, with its spinal segment receiving from the posterior circumflex humoral artery through the quadrilateral space, while the lateral and acromial segments receive from the acromial branch of the thoracoacromial artery [2].
During embryogenesis, the DM is formed from a mass of promyogenic cells that migrate from the dermomyotome toward the limb bud as early as 5-weeks’ gestation. This migrating mass of stem cells in the limb bud eventually splits into two, forming a collection on the ventral and dorsal side of the limb bud. The ventral mass of progenitors eventually becomes the flexors, pronators, and abductors, while the dorsal mass becomes the extensors and supinator’s of the upper limb, including the DM [3].
The DM was first described to be composed of seven different segments as early as 1734 by a German anatomist by the name of Bernhard Siegfried Albinus [4]. This claim was eventually reinforced by the works of more recent German scientists, in the biomechanical studies of the DM by Fick in 1811 [5] and the anatomical studies of Frohse and Fränkel in 1908 [6]. Newer technologies in biomechanics were used to further this idea using a mechanomyography study in 2007, further explaining the intricate control the brain has on the diverse cohort of actions of the DM. These studies provided evidence of the intricate distribution of both slow and fast-twitch muscle fibers that are distributed throughout the seven DM segments to offer gross and fine motor tuning of the DM across its complex control of the upper arm [7]. Intricate microdissection and study of the DM and its tendons at its origin and insertion give a detailed analysis of the morphological characteristics of these segments, providing even more information about the complex nature of this muscle [8].
With today’s surgical techniques trending toward a minimally invasive approach, there have been remarkable advances in limiting intra-operative iatrogenic injuries from previously openstyle surgeries. One of the most common procedures performed in the shoulder region is an arthroscopic rotator cuff repair. The anatomical location of the spinal segment of the DM carries the axillary nerve near points of surgical entry into the GHJ for repair [9]. It is important for surgeons and anesthetists alike to be aware of musculoskeletal variations in this region that could increase the risk for iatrogenic nerve injury.
Case Presentation
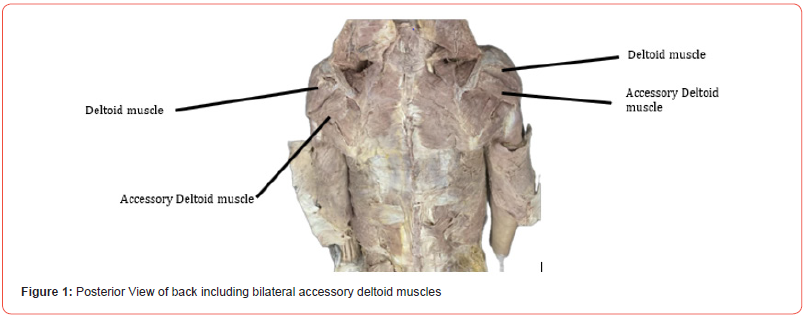
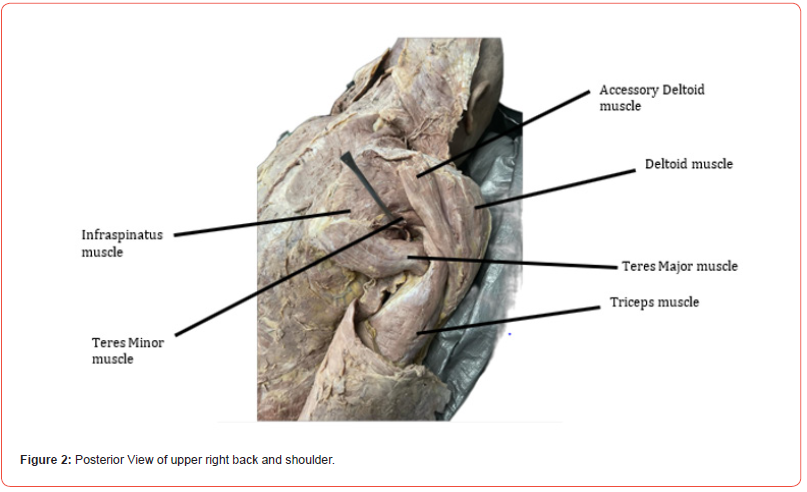
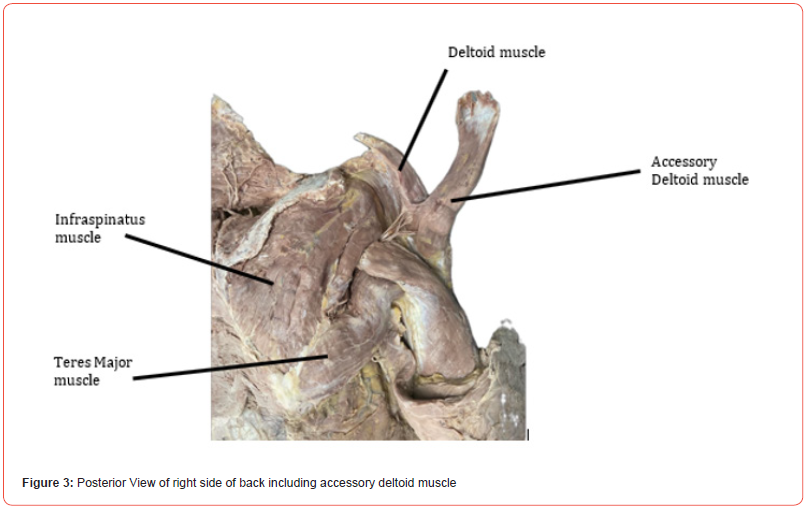
A case of bilateral accessory deltoid muscles which presented during routine dissection of a middle-aged male cadaver. The cadaver was received through the UNTHSC Willed Body Program. Upon dissection of the deltoid region, an unusual appearance and extension of the deltoid muscle was made apparent. The deltoid muscle seemed to be composed of two separate muscle groups, with one extending as far back and encompassing the entire spine of the scapula. After further dissection it was made clear that there were indeed two separate muscle groups of the deltoid, which were separated by a fascial layer. The main deltoid muscle was fed by the axillary nerve and posterior circumflex humeral artery. However, the accessory deltoid muscles had their own blood and nerve supply branching from the main deltoid supply. To validate this, we made sure to clearly dissect commonly found neighboring structures in the area, such as triceps, infraspinatus, supraspinatus, latissimus dorsi, trapezius, and rhomboids. After properly dissecting and identifying all these structures it was verified that this was indeed an accessory deltoid muscle. Once validated, dissection continued to the other deltoid region to conclude whether this was a unilateral or bilateral finding, and it was found to be bilateral finding. (Figures 1-3)
Discussion
In a full routine dissection of a middle-aged male cadaver, the spinal segment of the DM was found to be encased in its own fascial sheath bilaterally. Anatomical variations of the DM are not commonly reported in the literature. A case of a posterior DM segment encased in its own fascial compartment bilaterally has been reported, but only with no other anatomical variations [10]. Other reports describe it only being encased unilaterally with differing attachment sites to the scapula [11,12], with another describing its unilateral attachment to the infraspinatus fascia [13]. It has also been reported that the spinal segment of the deltoid had an accessory slip conjoining with the teres minor [14]. With the overall acceptance that the DM has seven separate mechanomyographic segments [7], it has been argued that these variants reported in the literature could in fact not be anatomical variants at all, although no formal classification system has been introduced [15]. Nevertheless, this DM variant is unique primarily for its concomitance with other anatomical variations. One of these variants presented as a split sciatic nerve through the piriformis, which could have led the donor to live a life with refractory sciatica [16]. Another variant in this same donor presented with a bilateral early splitting of the tibial nerve, at the level of the midgastrocnemius muscle. The overall relation of these concomitant variations, let alone their cause, remains largely unknown.
As all muscles require an attached nerve supply to maintain functionality, it is important to recognize the clinical significance of all anatomical variations in the musculature, and in this case, that of the posterior shoulder region. Peripheral nerves, particularly the axillary nerve, can be injured on posterior approach to the GHJ for open or arthroscopic rotator cuff repair [9]. In a systematic review of all post-operative complications from 19,262 reverse and anatomical shoulder arthroplasties, 0.4% (770 cases) had complications that were peripheral nerve injuries, with 70% of those nerve injuries being from a posterior surgical approach [17]. Not all nerve injuries arise from direct mechanisms such as transection or compression due to retraction, but could also arise from patient positioning, thermal injury from bone cement, or excessive edema or hematoma in the post-operative phase [18]. The risk of these complications could be increased in the setting of a vulnerable axillary nerve branch crossing under a seemingly separable space between fascial compartments of this DM variant’s lateral and spinal segments.
Targeted radiation therapy to the axilla to irradiate metastatic spread from breast cancers can cause radionecrotic ulcers that communicate to the GH joint [19]. DM muscle flaps originating from the spinal segment are used in these cases, in which the humeral insertion of the spinal segment is detached and rotated into the defect [19]. Misidentification of the DM variant could be confused for the teres major, causing unnecessary dissection of healthy tissue and resultant iatrogenic injury.
Although the primary focus of this discussion has been on the surgical implications for a DM variant presenting in this manner, it could also be significant in the procedural aspect of axillary nerve blocks by anesthesiologists. With the increasing use of diagnostic ultrasound and ultrasound guided procedures, deltoid tears concomitate with rotator cuff tears are being increasingly documented, requiring the need for more broad regional anesthesia for pain management [2]. In the setting of arthroscopic shoulder repair, suprascapular with axillary nerve blocks may be favorable over traditional interscalene brachial plexus blocks for patients with respiratory compromise [20]. The variant in the DM of this donor altered the course of normal axillary nerve anatomy, posing for the potential of misidentification during ultrasound guided axillary block.
Nerve injuries during shoulder procedures cause significant morbidity to the patient [21]. Although this DM variant did not present with a variation in nerve origin, its axillary nerve course to the muscle belly was altered due to its distinct fascial separation from the lateral segment. Reporting of musculoskeletal variants is important, primarily to educate the medical community about possible procedural complications and to inform on anatomical variation awareness to avoid iatrogenic injury.
Acknowledgement
The authors would like to thank the Willed Body Program at UNTHSC, the donors, and their families for their contribution to advancing medicine and anatomical knowledge.
Conflict of Interest
The authors have no conflicts of interest to disclose.
- Lambert SM (2020) Chapter 39: Shoulder girdle and upper arm. Gray’s Surgical Anatomy pp. 272-279.e3.
- Moser T, Junie Lecours, Johan Michaud, Nathalie J Bureau, Raphaël Guillin et al. (2013) The deltoid, a forgotten muscle of the shoulder. Skeletal Radiol 42(10): 1361-1375.
- Schoenwolf GC, Bleyl SB, Brauer PR, Francis-West PH (2021) Chapter 8: Development of the Musculoskeletal System. Larsen’s Human Embryology (6th Edition) pp. 166-190.
- Albinus BS (1734) Historiae musculorum Hominis. Leiden pp. 420-423.
- Fick R (1911) Handbuch der Anatomie und Mechanik der Gelenke. Fisher Verlag: Jena pp. 274-282.
- Frohse F, Fränkel M (1908) Die muskeln des menschlichen Armes. Fischer Verlag: Jena pp. 27-39.
- Gorelick ML, Brown JMM (2007) Mechanomyographic assessment of contractile properties within seven segments of the human deltoid muscle. Eur J Appl Physiol 100(1): 35-44.
- Leijnse JNAL, Han SH, Kwon YH (2008) Morphology of deltoid origin and end tondons- a generic model. J Anat 213(6): 733-742.
- Zhang J, Moore AE, and Stringer MD (2011) Iatrogenic upper limb nerve injuries: a systematic review. ANZ Journal of Surgery 81(4): 227-236.
- Kayikçioglu A, Celik HH, Yilmaz E (1993) An anatomic variation of the deltoid muscle (case report). Bull. De L’association Des Anat 77(238): 15-16.
- Kamburoğlu HO, Boran OF, Sargon MF, Keçik A (2008) An unusual variation of deltoid muscle. Int J Shoulder Surg 2(3): 62-63.
- Sawant SP, Shaik ST, More RM (2012) A variant deltoid muscle - A case report. Int J Cur Res Rev 4(19): 78-82.
- Gómez-Sánchez SM, Francisco Gómez-Esquer, Antonio Gil-Crujera, José Delcán-Giráldez, Gema Díaz-Gil et al. (2022) A Variant of the Deltoid Muscle and Its Clinical Implications: A Cadaveric Study. Anatomia 1(2): 119-125.
- Fraser PR, Thomas J, Guttman GD, Rosales AA (2014) Rare accessory slip of the deltoid muscle conjoined with teres minor. Eur J Anat 18(3): 195-197.
- Barbaix A (2008) Separate segments within the deltoid muscle: Anatomical variants or wishful thinking? Int J Shoulder Surg 2(3): 69-70.
- Ballout B, Van Alfen B, Ballout Y, Rosales A (2023) Bilateral Accessory Piriformis Variant and its Implications: A Case Report. Int J Anat Var 16(12): 439-441.
- Bohsali KI, Bois AJ, Wirth MA (2006). Current concepts review: complications of total shoulder arthroplasty. J Bone Joint Surg Am. 88(10): 2279-2292.
- Vajapey SP, Contreras ES, Cvetanovich GL, Neviaser AS (2021) Neurologic complications in primary anatomic and reverse total shoulder arthroplasty: A review. J of Clin Ortho and Trauma 20: 101475.
- Munnoch DA, Herbert KJ, Morris, AM, Stevenson JH (1996). The deltoid muscle flap: anatomical studies and case reports. British J of Plas Surg 49(5): 310-314.
- Sun C, Xiaofei Zhang, Xiaolin Ji, Peng Yu, Xu Cai et al. (2021) Suprascapular nerve block and axillary nerve block versus interscalene nerve block for arthroscopic shoulder surgery: a meta-analysis of randomized controlled trials. Medicine 100(44): e27661.
- Carofino BC David M Brogan, Michelle F Kircher, Bassem T Elhassan, Robert J Spinner et al. (2013) Iatrogenic Nerve Injuries During Shoulder Surgery. J of Bone & Joint Surg 95(18): 1667-1674.
-
Chase Green*, Bassam Ballout and Armando Rosales. An Atypical Variant of the Deltoid Muscle- A Case Report with Procedural Considerations. Anat & Physiol Open Access J. 1(4): 2024. APOAJ.MS.ID.000517.
-
Deltoid muscle; Variant; Fascia; Iatrogenic injury; Nerve injury; Axillary nerve block; Muscle flap; Shoulder surgery
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.